The relationship between medications and sleep is complex, often walking a fine line between therapeutic benefit and unintended consequences. Modern pharmacology offers numerous solutions for sleep disorders, yet these same compounds can sometimes create as many problems as they solve. Understanding how different drug classes interact with our natural sleep architecture requires examining both their mechanisms of action and their real-world effects on sleep quality and duration.
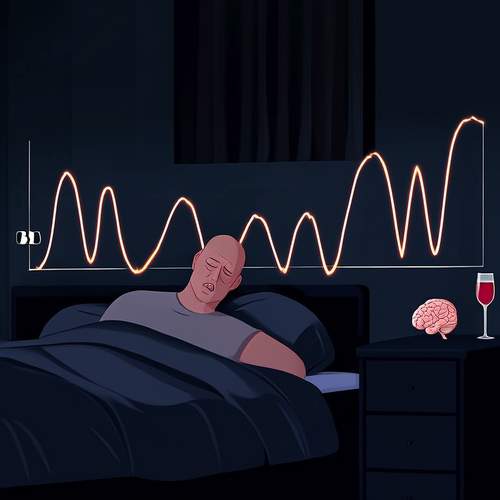
Prescription sleep aids dominate discussions about pharmaceutical sleep solutions, with benzodiazepines like temazepam and non-benzodiazepine "Z-drugs" such as zolpidem being among the most commonly prescribed. These medications primarily work by enhancing the effect of gamma-aminobutyric acid (GABA), the brain's main inhibitory neurotransmitter. While effective at initiating sleep, they often alter sleep architecture by reducing time spent in REM and deep sleep stages - the very phases crucial for cognitive restoration and memory consolidation. Many patients report feeling groggy or experiencing "hangover effects" the following morning, particularly with longer-acting formulations.
The antidepressant class of medications presents an interesting paradox in sleep pharmacology. While developed to treat mood disorders, many antidepressants significantly impact sleep patterns. Sedating tricyclics like amitriptyline were frequently prescribed off-label for insomnia before newer alternatives emerged. Modern selective serotonin reuptake inhibitors (SSRIs) often cause insomnia as a side effect during initial treatment, yet some patients eventually experience improved sleep as their underlying depression alleviates. The multifaceted relationship between depression, anxiety, and sleep means these medications can either disrupt or restore healthy sleep patterns depending on individual biochemistry and timing of administration.
Over-the-counter sleep remedies present their own set of considerations. Antihistamines like diphenhydramine, the active ingredient in many OTC sleep aids, induce drowsiness by blocking histamine receptors in the brain. While generally safe for occasional use, they can lead to tolerance with regular consumption and may cause next-day drowsiness or cognitive impairment, particularly in older adults. The American Geriatrics Society specifically recommends against using these medications in elderly patients due to increased risk of confusion, urinary retention, and falls.
Melatonin receptor agonists represent a more recent development in sleep pharmacology, with drugs like ramelteon targeting the body's natural sleep-wake cycle. Unlike traditional sedatives, these medications work by mimicking the action of melatonin, the hormone our brains produce in response to darkness. While generally well-tolerated with minimal next-day effects, their efficacy varies significantly between individuals. Some patients report dramatic improvements in sleep onset latency, while others notice little effect. The delayed onset of action (typically taking several weeks for full effect) also makes them less suitable for acute insomnia cases.
The impact of stimulant medications on sleep deserves particular attention, especially considering their widespread use for ADHD and narcolepsy. Drugs like methylphenidate and amphetamine derivatives can significantly delay sleep onset if taken too late in the day. Paradoxically, when properly dosed and timed, these medications may actually improve sleep quality in ADHD patients by reducing the racing thoughts and restlessness that often prevent them from falling asleep. The key lies in finding the optimal dosing schedule that provides daytime symptom control without interfering with nocturnal sleep patterns.
Chronic pain medications present another complex interaction with sleep. Opioids, while effective at pain management, frequently disrupt sleep architecture by increasing light sleep at the expense of restorative deep sleep stages. Many patients on long-term opioid therapy report poor sleep quality despite adequate pain control. Nonsteroidal anti-inflammatory drugs (NSAIDs) may offer a better alternative for pain-related sleep disturbances, though their potential gastrointestinal and cardiovascular risks limit long-term use. The search for pain relief that doesn't compromise sleep quality remains an ongoing challenge in clinical practice.
Blood pressure medications, particularly beta blockers, demonstrate how drugs targeting completely different body systems can influence sleep. These cardiovascular medications frequently cause vivid dreams and nighttime awakenings, with some patients reporting bizarre or disturbing dream content. The mechanism appears related to suppression of melatonin production, though the exact pathways remain under investigation. For patients experiencing these side effects, switching to morning dosing or alternative antihypertensive classes often resolves the sleep disturbances without compromising blood pressure control.
The emerging field of orexin receptor antagonists offers promising new directions in sleep pharmacology. Drugs like suvorexant work by temporarily blocking wake-promoting orexin neurotransmitters rather than broadly depressing central nervous system activity. Early research suggests these medications may preserve more natural sleep architecture compared to traditional sedatives, with potentially lower risks of dependence and next-day impairment. However, their long-term effects and optimal use patterns require further study as these relatively new entrants to the sleep aid market.
Perhaps most concerning in sleep pharmacology is the issue of dependence and withdrawal. Many prescription sleep medications, particularly benzodiazepines and Z-drugs, can lead to physical dependence with prolonged use. Withdrawal symptoms often include rebound insomnia worse than the original sleep problem, creating a vicious cycle of continued use. Cognitive behavioral therapy for insomnia (CBT-I) has emerged as an effective non-pharmacological alternative, though access to trained practitioners remains limited in many areas. The ideal approach often involves using medications short-term while developing sustainable behavioral strategies for long-term sleep health.
Individual variation in drug metabolism further complicates the medication-sleep equation. Genetic differences in liver enzyme activity mean the same dose of a sleep medication can produce dramatically different effects between patients. A dose that leaves one person groggy the next morning might be completely ineffective for another. Pharmacogenetic testing holds promise for personalizing sleep medication choices, though cost and availability currently limit widespread adoption of this approach.
The future of sleep pharmacology likely lies in more targeted therapies that address specific sleep disturbances without broadly affecting consciousness. Research into adenosine receptors, circadian rhythm regulators, and specific neurotransmitter systems may yield medications that can be tailored to individual sleep architecture disturbances. For now, the most prudent approach combines judicious short-term medication use with sleep hygiene optimization, light exposure management, and behavioral interventions to address the root causes of sleep disturbances rather than just their symptoms.
As our understanding of sleep neurobiology deepens, so too will our pharmacological tools for managing sleep disorders. The challenge lies in developing interventions that work with, rather than against, the brain's natural sleep mechanisms. Until that ideal is realized, medications will remain both valuable tools and potential pitfalls in the ongoing pursuit of restorative sleep.

By /May 22, 2025

By /May 22, 2025

By /May 22, 2025
By /May 22, 2025
By /May 22, 2025

By /May 22, 2025
By /May 22, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025