Gender and Sleep: Exploring the Biological and Social Differences
Sleep is a fundamental human need, yet the way men and women experience it can differ significantly. Research has shown that gender plays a crucial role in sleep patterns, quality, and disorders. From biological factors like hormones to social roles and stress levels, the interplay between gender and sleep is complex and often overlooked. Understanding these differences can lead to better health outcomes and more personalized approaches to sleep medicine.
The Biological Divide: Hormones and Sleep Architecture
One of the most significant factors influencing sleep differences between genders is biology. Women, for instance, experience hormonal fluctuations throughout their menstrual cycles, pregnancy, and menopause, all of which can disrupt sleep. Estrogen and progesterone, the primary female sex hormones, have been linked to sleep regulation. Lower levels of these hormones, particularly during menopause, often lead to insomnia and restless nights. Men, on the other hand, tend to have more stable hormonal profiles, though declining testosterone levels in older age can also affect sleep quality.
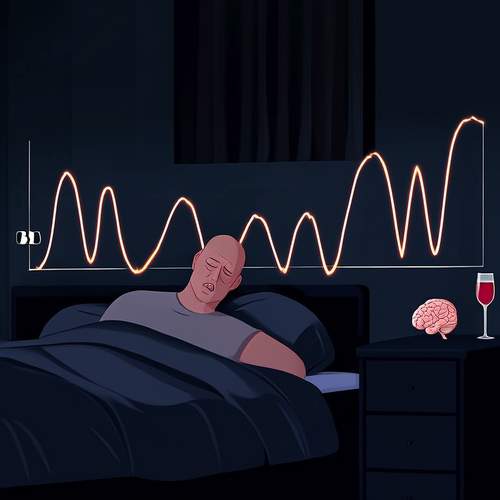
Sleep architecture—the structure of the sleep cycle—also varies between genders. Studies suggest that women spend more time in deep sleep stages, which are critical for physical restoration. However, they are also more prone to frequent awakenings, leading to fragmented sleep. Men, while sleeping more soundly in some cases, are more likely to suffer from sleep apnea, a condition linked to anatomical differences such as wider neck circumferences and airway structures.
Social Roles and Sleep Disruptions
Beyond biology, societal expectations and lifestyle factors contribute to sleep disparities. Women often juggle multiple roles—caregivers, professionals, and homemakers—which can lead to heightened stress and anxiety, both of which are notorious sleep disruptors. The mental load of managing household responsibilities, even in dual-income households, frequently falls disproportionately on women, cutting into their sleep time and quality.
Men, while generally reporting fewer sleep interruptions, face their own set of challenges. Societal pressures to embody traditional masculinity can discourage men from seeking help for sleep issues or admitting fatigue. This reluctance to address sleep problems can exacerbate conditions like insomnia or sleep apnea, leading to long-term health consequences such as cardiovascular disease or diabetes.
Sleep Disorders: A Gendered Perspective
Certain sleep disorders manifest differently across genders. For example, women are twice as likely as men to suffer from insomnia, a condition often tied to anxiety and hormonal changes. Restless legs syndrome, another sleep disorder, is also more prevalent among women, particularly during pregnancy. On the flip side, men are more frequently diagnosed with obstructive sleep apnea, a condition that not only disrupts sleep but also increases the risk of heart disease and stroke.
Interestingly, the symptoms of these disorders can present differently based on gender. Women with sleep apnea, for instance, may report fatigue or depression rather than the classic snoring and gasping for air seen in men. This discrepancy can lead to underdiagnosis or misdiagnosis, highlighting the need for gender-sensitive approaches in sleep medicine.
Cultural Influences and Coping Mechanisms
Cultural norms further shape how men and women approach sleep. Women are more likely to use relaxation techniques or seek medical advice for sleep troubles, while men may turn to alcohol or overwork as coping mechanisms—both of which can worsen sleep quality. The stigma around vulnerability in men often prevents them from adopting healthier sleep habits, whereas women may feel more permitted to prioritize self-care but struggle to find the time amid caregiving duties.
These cultural dynamics extend to bedtime routines as well. Women often report winding down with reading or meditation, while men might stay up later engaging in stimulating activities like video games or watching TV. Such habits can either promote or hinder restful sleep, depending on their nature and timing.
Toward Better Sleep for All
Addressing sleep disparities requires a multifaceted approach. Medical professionals must consider gender when diagnosing and treating sleep disorders, recognizing that symptoms and risk factors may differ. Public health campaigns should raise awareness about the importance of sleep hygiene while challenging societal norms that discourage men from seeking help or women from prioritizing their own rest.
On an individual level, both men and women can benefit from establishing consistent sleep schedules, creating restful environments, and managing stress through mindfulness or therapy. Employers, too, play a role by fostering workplace cultures that respect work-life balance and discourage the glorification of sleep deprivation as a badge of productivity.
Ultimately, sleep is not a one-size-fits-all experience. By acknowledging and addressing the unique challenges faced by different genders, we can move closer to a world where everyone has the opportunity to enjoy restorative, high-quality sleep.

By /May 22, 2025

By /May 22, 2025

By /May 22, 2025
By /May 22, 2025
By /May 22, 2025

By /May 22, 2025
By /May 22, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025