Cognitive Behavioral Therapy for Insomnia: Rewiring the Restless Mind
The moon hangs high, the world falls silent, yet millions find themselves trapped in the exhausting cycle of sleeplessness. Insomnia isn't just about counting sheep or drinking warm milk—it's often rooted in deeply ingrained thought patterns that sabotage our ability to rest. Cognitive Behavioral Therapy for Insomnia (CBT-I) has emerged as a groundbreaking approach that doesn't just treat the symptoms but rewires the very mechanisms of sleeplessness.
Unlike sleeping pills that provide temporary relief, CBT-I targets the psychological and behavioral components fueling insomnia. The therapy operates on a simple yet profound principle: our thoughts about sleep directly impact our ability to sleep. When someone lies awake at night thinking "I'll never fall asleep" or "I'll be useless tomorrow," these catastrophic predictions become self-fulfilling prophecies. CBT-I helps break this vicious cycle by challenging and restructuring these maladaptive beliefs.
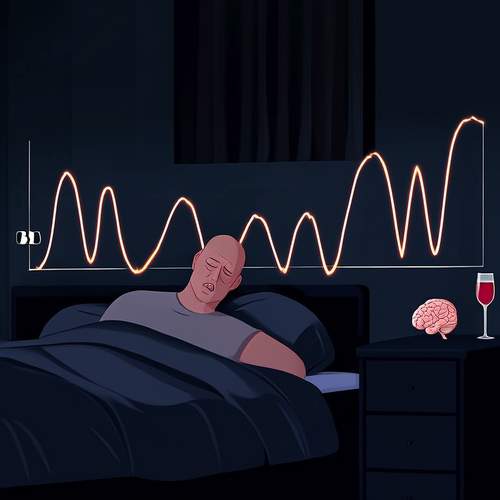
The sleep restriction component of CBT-I often surprises patients. Rather than spending more time in bed trying to catch up on lost sleep, therapists actually prescribe less time in bed initially. This creates mild sleep deprivation that helps rebuild the body's natural sleep drive. As sleep efficiency improves, the time in bed is gradually increased. This counterintuitive approach proves more effective than the common instinct to sleep late or nap after a bad night.
Another cornerstone of CBT-I involves stimulus control—reassociating the bed with sleep rather than frustration. Patients learn to use their beds only for sleep and intimacy, avoiding activities like watching TV or working in bed. If unable to sleep after 20 minutes, they're instructed to get up and engage in a quiet activity until feeling sleepy again. This helps break the conditioned anxiety many develop toward their own bedrooms.
Perhaps the most transformative aspect of CBT-I is its focus on cognitive restructuring. Insomniacs often develop irrational beliefs about sleep ("I must get eight hours or I'll get sick") or catastrophic thinking about the consequences of poor sleep. Therapists guide patients to examine the evidence for these beliefs and develop more balanced perspectives. Many discover that their feared outcomes rarely materialize, even after poor sleep.
The effectiveness of CBT-I isn't just anecdotal. Research shows it helps approximately 70-80% of people with primary insomnia, with benefits often lasting years after treatment. Unlike medications, there are no side effects beyond temporary sleepiness during the initial adjustment period. The therapy has proven particularly helpful for groups prone to insomnia like menopausal women, cancer patients, and older adults.
Implementing CBT-I requires commitment and patience. The first weeks can be challenging as patients adjust to new sleep schedules and confront long-held beliefs about sleep. Many report feeling sleepier initially as their bodies adapt. However, those who persist typically begin noticing improvements within 3-4 weeks. The skills learned become lifelong tools for maintaining healthy sleep, making CBT-I a truly sustainable solution.
As sleep science advances, CBT-I continues evolving. Digital platforms now offer guided CBT-I programs, making the treatment more accessible. Some therapists incorporate mindfulness techniques to help patients observe their sleep-related thoughts without reacting to them. These innovations build on the core principles while adapting to modern lifestyles.
The quiet revolution of CBT-I offers hope to those trapped in the exhausting cycle of sleepless nights. By addressing the root cognitive and behavioral causes rather than just symptoms, it provides what sleeping pills cannot—a lasting peace treaty with the night. In our overstimulated world, the ability to sleep soundly may be one of the most valuable skills we can cultivate, and CBT-I offers a scientifically validated path to reclaiming the night.

By /May 22, 2025

By /May 22, 2025

By /May 22, 2025
By /May 22, 2025
By /May 22, 2025

By /May 22, 2025
By /May 22, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025